 Dr. Joseph Mele is dedicated to fostering improvement, not just in his patients, but in the basic science that is the foundation of Plastic Surgery. Dr. Mele participated in the original Silicone Breast Implants Adjunct Studies for both US breast implant manufacturers at the time: Allergan and Mentor These investigations into the safety and effectiveness of Silicone Breast Implants, eventually led to their FDA approval after years of restricted use. He continues to be a Primary Investigator for all three current US FDA approved manufacturers of breast implants: Sientra, Allergan and Mentor. By participating in these long-term follow-up studies, Dr. Mele continues to demonstrate his commitment to Patient Safety and predictable plastic surgery results.
Dr. Joseph Mele is dedicated to fostering improvement, not just in his patients, but in the basic science that is the foundation of Plastic Surgery. Dr. Mele participated in the original Silicone Breast Implants Adjunct Studies for both US breast implant manufacturers at the time: Allergan and Mentor These investigations into the safety and effectiveness of Silicone Breast Implants, eventually led to their FDA approval after years of restricted use. He continues to be a Primary Investigator for all three current US FDA approved manufacturers of breast implants: Sientra, Allergan and Mentor. By participating in these long-term follow-up studies, Dr. Mele continues to demonstrate his commitment to Patient Safety and predictable plastic surgery results.
Dr. Mele’s research has been recognized by his peers. He has presented original research at national, state and local plastic surgery meetings, and has published articles related to Cosmetic Plastic Surgery including, but not limited to, Scar Minimization, Patient Safety and Plastic Surgery Resident Training, in the most respected, peer-reviewed, US Plastic Surgery Journals including:
- Aesthetic Plastic Surgery – The Official Journal of the International Society of Aesthetic Plastic Surgery (ISAPS); the European Association of Societies of Aesthetic Plastic Surgery (EASAPS), the Sociedade Brasileira de Cirurgia Plastica (SBCP), and the Società Italiana di Chirurgia Plastica Ricostruttiva ed Estetica (SICPRE).
- Plastic and Reconstructive Surgery (aka The White Journal) – The Official Journal of the American Society of Plastic Surgeons (ASPS) – This is the most respected US Journal dedicated to General Plastic and Reconstructive Surgery and the official publication of the largest association of Plastic Surgeons in the US, if not the world.
- The Annals of Plastic Surgery – This is the only independent journal devoted to General Plastic and Reconstructive Surgery.
- The Journal of Burn Care & Rehabilitation (now The Journal of Burn Care & Research) – The Official Journal of the American Burn Association (ABA) – This is the only US journal devoted exclusively to the treatment and rehabilitation of patients with burns.
Dr. Mele’s Plastic Surgery Research & Publications Article Titles and Links to More
Here are a list of some of the Plastic Surgery Research articles that Dr. Mele has published. For more detailed information about each articles, just click on the title:
- A Randomized Controlled Trial of the Embrace Advanced Scar Therapy Device to Reduce Incisional Scar Formation
- Suspension Technique for Panniculectomy in a Morbidly Obese Patient
- Laser Blepharoplasty: Is It Safe?
- HIV Seropositivity In a Burn Center’s Population
- Treatment of Thromboembolic Complications of Fulminant Meningococcal Septic Shock
- Chronic Hyperpigmentation From a Heated Mustard Compress Burn: A Case Report
- Teaching Aesthetic Surgery at the Resident Level
- The Effect of Antenatal Surgery on Craniofacial Growth in Sheep Model
Dr. Mele’s Plastic Surgery Research & Publications: Abstracts and More Information for Each Article
A Randomized Controlled Trial of the Embrace Advanced Scar Therapy Device to Reduce Incisional Scar Formation
 A Randomized Controlled Trial of the Embrace Advanced Scar Therapy Device to Reduce Incisional Scar Formation.
A Randomized Controlled Trial of the Embrace Advanced Scar Therapy Device to Reduce Incisional Scar Formation.
Longaker MT, Rohrich RJ, Greenberg L, Furnas H, Wald R, Bansal V, Seify H, Tran A, Weston J, Korman JM, Chan R, Kaufman D, Dev VR, Mele JA, Januszyk M, Cowley C, McLaughlin P, Beasley B, Gurtner GC.
Department of Surgery, Division of Plastic and Reconstructive Surgery, Stanford University School of Medicine, 291 Campus Drive, Stanford, CA, 94305
Plast Reconstr Surg. 2014 Sep;134(3):536-46. doi: 10.1097/PRS.0000000000000417.
BACKGROUND: Scarring represents a significant biomedical burden in clinical medicine. Mechanomodulation has been linked to scarring through inflammation, but until now a systematic approach to attenuate mechanical force and reduce scarring has not been possible.
METHODS: The authors conducted a 12-month, prospective, open-label, randomized, multicenter clinical trial to evaluate abdominoplasty scar appearance following postoperative treatment with the embrace Advanced Scar Therapy device to reduce mechanical forces on healing surgical incisions. Incisions from 65 healthy adult subjects were randomized to receive embrace treatment on one half of an abdominoplasty incision and control treatment (surgeon’s optimal care methods) on the other half. The primary endpoint for this study was the difference between assessments of scar appearance for the treated and control sides using the visual analogue scale scar score.
RESULTS: Final 12-month study photographs were obtained from 36 subjects who completed at least 5 weeks of dressing application. The mean visual analogue scale score for embrace-treated scars (2.90) was significantly improved compared with control-treated scars (3.29) at 12 months (difference, 0.39; 95 percent confidence interval, 0.14 to 0.66; p = 0.027). Both subjects and investigators found that embrace-treated scars demonstrated significant improvements in overall appearance at 12 months using the Patient and Observer Scar Assessment Scale evaluation (p = 0.02 and p less than 0.001, respectively). No serious adverse events were reported.
CONCLUSIONS: These results demonstrate that the embrace device significantly reduces scarring following abdominoplasty surgery. To the authors’ knowledge, this represents the first level I evidence for postoperative scar reduction.
Suspension Technique for Panniculectomy in a Morbidly Obese Patient
 Suspension Technique for Panniculectomy in a Morbidly Obese Patient.
Suspension Technique for Panniculectomy in a Morbidly Obese Patient.
Linder SA, Buncke GM, Cooper T, Mele JA, Kind GM, Buncke HJ.
Division of Plastic and Reconstructive Surgery, The Buncke Clinic, Davies Medical Center, 45 Castro Street, San Francisco, California, USA, 94114.
Contemporary Surgery. 2011 March 10.
ABSTRACT: A simplified technique for removal of a large pannus is described. The case presented involves a 63-year old morbidly obese man (more than 500 pounds) with multiple medical problems. Complications encountered when operating on the morbidly obese because of the sheer size of the patient and the body part to be operated on are briefly discussed. Two operating tables were necessary to accommodate the patient’s large bulk. Preparation of the skin as well as the operative procedure were greatly facilitated by using a hydraulic lift to elevate the pannus. No injuries were sustained by the surgeons of the operating room staff. Total operative time was 2.5 hours, and there were no intraoperative or postoperative complications. This technique may be used to perform other procedures in the morbidly obese that require elevation of a body part.
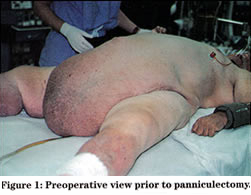 INTRODUCTION: A 63-year old morbidly obese male (estimated weight: 515 pounds) was admitted for surgical correction of an enormous pannus. Indications for panniculectomy included mechanical compression of the lower extremity lower venous system, lower abdominal hygiene, and decreased mobility. The patient initially was admitted to the cardiology service with multiple medical problems associated with his morbid obesity including congestive heart failure, atrial fibrillation, and marked chronic venous stasis of the lower extremities. On examination, the abdominal pannus and lower legs appeared markedly lymphadematous. Preoperative medical workup included pulmonary function tests, echocardiogram, and upper and lower gastrointestinal endoscopy for investigation of microcytic anemia. With aggressive preoperative diuresis, a weight loss of 45 pounds was achieved.
INTRODUCTION: A 63-year old morbidly obese male (estimated weight: 515 pounds) was admitted for surgical correction of an enormous pannus. Indications for panniculectomy included mechanical compression of the lower extremity lower venous system, lower abdominal hygiene, and decreased mobility. The patient initially was admitted to the cardiology service with multiple medical problems associated with his morbid obesity including congestive heart failure, atrial fibrillation, and marked chronic venous stasis of the lower extremities. On examination, the abdominal pannus and lower legs appeared markedly lymphadematous. Preoperative medical workup included pulmonary function tests, echocardiogram, and upper and lower gastrointestinal endoscopy for investigation of microcytic anemia. With aggressive preoperative diuresis, a weight loss of 45 pounds was achieved.
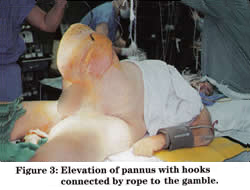
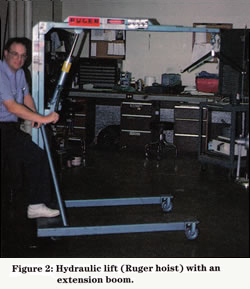 METHODS: Intraoperative monitoring was performed using an arterial line and a Swan-Ganz catheter. Two operating tables were necessary to accommodate the patient’s bulk (see Figure 1 above). Preparation of the skin and the operative procedure were greatly facilitated by using a hydraulic lift to elevate the pannus. With assistance from the biomedical engineering department, two intramedullary rods (1/4-inch stainless steel) were bent into lifting hooks. The “Ruger hoist” included an extension book with variable standing positions (450, 750, and 1000 pounds) determined by its length (Figure 2). In order to gain maximum extension of the boom for positioning at the side of the surgical table, a total weight of 450 pounds could be elevated safely. The hooks were connected by rope to a gamble mounted on the hydraulic lift (Figure 3).
METHODS: Intraoperative monitoring was performed using an arterial line and a Swan-Ganz catheter. Two operating tables were necessary to accommodate the patient’s bulk (see Figure 1 above). Preparation of the skin and the operative procedure were greatly facilitated by using a hydraulic lift to elevate the pannus. With assistance from the biomedical engineering department, two intramedullary rods (1/4-inch stainless steel) were bent into lifting hooks. The “Ruger hoist” included an extension book with variable standing positions (450, 750, and 1000 pounds) determined by its length (Figure 2). In order to gain maximum extension of the boom for positioning at the side of the surgical table, a total weight of 450 pounds could be elevated safely. The hooks were connected by rope to a gamble mounted on the hydraulic lift (Figure 3).
 The total operative time was 2.5 hours, and there were no intraoperative complications. Equally important, no injuries occurred to either the operating room staff or the surgeons in association with the physical difficulty of maneuvering a morbidly obese patient intraoperatively. The entire operative specimen weighed 100 pounds. The estimated blood loss was approximately 450cc. The patient received one unit of packed red blood cells and two liters of crystalloid intraoperatively. No further transfusions were required. There were no postoperative complications. The patient was extubated with removal of a central line on the second postoperative day. Embolic prophylaxis with subcutaneous heparin was administered for five days until ambulation. Unna’s boots were placed on the lower extremities every three days to aid in the reduction of edema and as a treatment for chronic venous ulcerations. After one week, the patient was transferred to a skilled nursing facility from which he was discharged on postoperative day 13.
The total operative time was 2.5 hours, and there were no intraoperative complications. Equally important, no injuries occurred to either the operating room staff or the surgeons in association with the physical difficulty of maneuvering a morbidly obese patient intraoperatively. The entire operative specimen weighed 100 pounds. The estimated blood loss was approximately 450cc. The patient received one unit of packed red blood cells and two liters of crystalloid intraoperatively. No further transfusions were required. There were no postoperative complications. The patient was extubated with removal of a central line on the second postoperative day. Embolic prophylaxis with subcutaneous heparin was administered for five days until ambulation. Unna’s boots were placed on the lower extremities every three days to aid in the reduction of edema and as a treatment for chronic venous ulcerations. After one week, the patient was transferred to a skilled nursing facility from which he was discharged on postoperative day 13.
DISCUSSION: The pathophysiology of Panniculus Morbidus was described by Petty et all in 19921. A large pannus creates a vicious cycle of lymphatic and venous congestion leading to further ischemia and lymphedema, ultimately resulting in cellulitis, abscess formation, and infarction. During surgical dissection, it was evident that this patient has a markedly lymphadematous pannus. Surgery in the obese patient has been associated with an increased incidence of complications and mortality including deep vein thrombosis, pulmonary embolism, pneumonia, sepsis, and would dehiscence with fat/skin necrosis. Obesity is commonly defined as being more than 20% over the ideal body weight; morbid obesity is defined as being more than twice the ideal body weight. In a review of the literature published in 1985, Hirsch et al2 found a variable, but nonetheless high (20-78%), incidence of complications following surgery in the morbidly obese patient. Abdel-Moneim noted a 2.6% mortality rate from surgery in obese patients.3 According to Foley and Lee4 the incidence of wound infections in morbidly obese patients is as high as 40%, and would dehiscence is ten times more likely to occur in this patient population. Reducing operative time may decrease the incidence of would sepsis, would dehiscence, and hernia formation. Various techniques have been described to aid in suspension of the pannus. Richards described placement of a rigid bar through the pannus to provide suspension and enhance manipulation.5 Meyerowitz et al described the transverse placement of Rush nails for suspension.6 The skewered Rush nail method has been modified by bending the intramedullary rods into hooks. Sterilized “shark hooks” also could be used easily. Matory et al7 described a pannus elevation technique using rope suspension with towel clips and Steinmann pins. The method of suspension used in this case allows complete surgical resection of the pannus without requiring multiple assistants. The hydraulic lift boom was extended to its greatest length to maintain the sterile field. The nurse controlled the manual pump that is used to elevate the pannus on the hoist. Our biomedical engineers recommended using a thicker rod, at least 3/8-inch in diameter, to prevent the bending that was evident with the 1/4 inch rod.
CONCLUSION: The technique describes for panniculectomy will expedite the operation, reduce blood loss, and optimize the volume and venous return. Visualization of the vessels is easier and hemostasis is more readily accomplished with reduced blood loss. Prevention of injury to the operating room staff and surgeons also is an important consideration.
REFERENCES:
1 Petty P, Mandon PN, Black R, et al: Panniculus morbidus. Ann Plast Surg 28:442-454, 1992.
2 Hirsch J, et al: Health implications of obesity: NIH Consensus Development Conference statement. Ann Intern Med 103:1073, 1985.
3 Abdel-Moneim RI: The hazards of surgery in the obese. Int Surg 70:101, 1985.
4 Foley K, Lee R: Surgical complications of obese patients with endometrial carcinoma. Gynecol Oncol 39:171, 1990.
5 Richards EF: A mechanical aid for abdominal panniculectomy. Br J Plast Surg 18:336, 1965.
6 Meyerowitz BR, Gruber RP, Laub DR, et al: Massive abdominal panniculectomy. JAMA 225:408, 1973.
7 Matory WE, O’Sullivan J, Fudem G, Dunn R: Abdominal surgery in patients with severe morbid obesity. Plast Reconstr Surg 94:976:987, 1994.
Laser Blepharoplasty: Is It Safe?
 Laser Blepharoplasty: Is It Safe?
Laser Blepharoplasty: Is It Safe?
Mele JA, Kulick MI, Lee D
Division of Plastic and Reconstructive Surgery, Saint Francis Memorial Hospital, 900 Hyde St, San Francisco, CA, USA, 94109.
Aesthetic Plast Surg. 1998 Jan-Feb;22(1):9-11.
ABSTRACT: The complications of the “traditional” blepharoplasty have been well outlined; however, very little can be found on the safety of lasers when used for blepharoplasty. In this article, 20 consecutive patients undergoing laser blepharoplasty are examined preoperatively and postoperatively for eye function and ocular injury by an independent ophthalmologist. Follow-up examinations were performed at random times after surgery ranging from 4 to 60 days, with the majority of patients (17 of 20) seen between 4 and 17 days after surgery. Any changes from the preoperative examinations were recorded. Results demonstrated no complications associated with the use of lasers during blepharoplasty. Safety precautions and surgical procedures are outlined. An attempt is made to separate those hazards specific to the laser technique from the “traditional” blepharoplasty procedure.
HIV Seropositivity In a Burn Center’s Population
 HIV Seropositivity In a Burn Center’s Population
HIV Seropositivity In a Burn Center’s Population
Mele JA, Linder SA, Calabria R, Ikeda CJ.
Division of Plastic and Reconstructive Surgery, Bothin Burn Unit, Saint Francis Memorial Hospital, 900 Hyde St, San Francisco, CA, USA, 94109..
J Burn Care Rehabil. 1998 Mar-Apr;19(2):138-41.
ABSTRACT: HIV infection in a patient with burn injuries complicates the care of both the patient and the treating burn team. In the patient, HIV slows wound healing and increases the complications seen with burns. For the treating team, HIV is a hazard that infects the large volume of bodily fluids to which the burn team is potentially exposed. At Saint Francis Memorial Hospital, a team of plastic surgeons, infectious disease specialists, medical internists, psychiatrists, social workers, and nurses was established for the care of patients with burn injuries who have HIV. To ascertain the baseline need for this specialized care, we interviewed 103 consecutive patients admitted to the Bothin Burn Center. Those found to be positive by history (3 of 103) were excluded from HIV testing. Of the remaining 100 consecutive patients, all consented to HIV testing. None of these patients, even those with known risk factors, was found to have undiagnosed HIV positivity. We conclude the occult incidence in the population tested is lower than expected, and continued testing is warranted.
Treatment of Thromboembolic Complications of Fulminant Meningococcal Septic Shock
 Treatment of Thromboembolic Complications of Fulminant Meningococcal Septic Shock
Treatment of Thromboembolic Complications of Fulminant Meningococcal Septic Shock
Mele JA, Linder S, Capozzi A.
Department of Plastic and Reconstructive Surgery, Bothin Burn Center, Saint Francis Memorial Hospital, 900 Hyde St, San Francisco, CA, USA, 94109.
Ann Plast Surg. 1997 Mar,38(3):283-90. Review.
ABSTRACT: A patient report of fulminant meningococcal septic shock is described. The presentation, hospital course, and reconstructive efforts are outlined, and a brief review of meningococcal infection is included. Emphasis is placed on the algorithm used to determine treatment. A 19-year-old Hispanic male presented with all the hallmarks of Waterhouse-Friderichsen syndrome (WFS)-sudden onset, high fever, dyspnea with intermittent cyanosis, shock, disseminated intravascular coagulopathy, and the development of purpura. The pathognomonic feature of WFS-hemorrhage into the adrenal glands-if present, was not extensive, as he did not require steroid supplementation. Though cerebrospinal fluid latex agglutination was negative, his serum was positive for group C Neisseria and admission blood cultures grew Neisseria meningitidis. Thromboembolic complications were systemic with the highest morbidity peripherally in the lower extremities. Care for these injuries involved every rung of the reconstructive ladder-from local wound care and skin grafts to local flaps and microvascular transplantation.
Chronic Hyperpigmentation From a Heated Mustard Compress Burn: A Case Report
 Chronic Hyperpigmentation From a Heated Mustard Compress Burn: A Case Report
Chronic Hyperpigmentation From a Heated Mustard Compress Burn: A Case Report
Linder SA, Mele JA, Harries T.
Department of Plastic and Reconstructive Surgery, Bothin Burn Center, Saint Francis Memorial Hospital, 900 Hyde St, San Francisco, CA, USA, 94109.
J Burn Care Rehabil. 1996 Jul-Aug;17(4):351-2. Review.
ABSTRACT: This is a case study of a woman who sustained a second-degree, partial-thickness burn of the midchest and medial breast distribution after the application of a heated mustard compress as a naturopathic remedy for a recent bout of pneumonia. This case study demonstrates the potential for hyperpigmentation and hypertrophic scarring associated with heated mustard burns. A photograph of the presenting burn with the region of hyperpigmentation 3 days after the injury is provided.
Teaching Aesthetic Surgery at the Resident Level
 Teaching Aesthetic Surgery at the Resident Level
Teaching Aesthetic Surgery at the Resident Level
Linder SA, Mele JA, Capozzi A.
Department of Plastic Surgery, St. Francis Memorial Hospital, 900 Hyde St, San Francisco, CA, USA, 94109.
Aesthetic Plast Surg. 1996 Jul-Aug;20(4):351-4.
ABSTRACT: The field of plastic and reconstructive surgery continues to broaden its scope while other fields continue to narrow theirs. The inability to teach aesthetic surgery is often confounded by the absence of an aesthetic surgery clinic for the chief resident, a reduced number of procedures and cases available, and a lack of faculty staff involvement. A close examination of the 19 western United States-based plastic surgery programs was performed in order to determine the most useful methods in teaching aesthetic surgery. An aesthetic surgery survey was distributed to most recently graduated plastic surgery residents to evaluate their overall experience in aesthetic surgery during residency. Of the 40 residents’ surveys, 31 were returned. As anticipated, greater than half (51.6%) of the western United States programs were without a chief resident aesthetic clinic. Also, greater than half of those surveyed (51.6%) felt that the quantity of aesthetic cases was insufficient. The residents’ comfort in performing specific operations was quite variable. From data analysis it is apparent there is a greater requirement for “hands-on” experience with aesthetic surgical cases during residency training. Overwhelmingly, the responses indicated the need for a Chief Resident Aesthetic Clinic, greater faculty involvement, and an increased clinic population with attending staff assistance. A 6-month chief resident aesthetic surgery clinic rotation at Saint Francis Memorial Hospital has proven to be very beneficial in teaching all aspects including pre-operative evaluation, surgical technique, and postoperative care of the aesthetic patient.
The Effect of Antenatal Surgery on Craniofacial Growth in Sheep Model
 The Effect of Antenatal Surgery on Craniofacial Growth in Sheep Model
The Effect of Antenatal Surgery on Craniofacial Growth in Sheep Model
Thaller SR, Mele J, Hoyt J.
Division of Plastic Surgery, University of California Davis Medical Center, 2315 Stockton Blvd, Sacramento, CA, USA, 95817.
Plast Reconstr Surg. 1995 Jul;96(1):1-8.
ABSTRACT: The purpose of this investigation was to evaluate the effect of antenatal palatal surgery in a sheep model. At 75 to 90 days of gestation, 20 fetuses underwent surgical in utero manipulation of their palates with the incision and elevation of bilateral bipedicled mucoperiosteal flaps. Sixteen of the 20 sheep (80 percent) went on to a normal full-term delivery. The palates and facial appearances were grossly evaluated, and detailed measurements were made of the palates. The data underwent statistical analysis. We were unable to discern any differences between the experimental group and the age-matched controls. Antenatal palatal surgery appeared to have no effect on craniofacial growth and development.